June is World Infertility Awareness Month!
According to the CDC, about 6% of married women aged 15 to 44 years in the United States are unable to get pregnant after one year of trying—this is infertility. In honor of infertility awareness month, I think it is finally time to share our story. I am so excited to be able to share it with you, our dear readers.
So, hold on tight: this is a bit of a long one!
The start of our baby book began several years ago. It began with me coming off birth control and not really worrying. After about 6 months of unsuccessfully trying, I began to track my cycles more closely. I always knew I had inconsistencies but did not realize the extent. I had always had painful periods and suspected there may be issues. Basic testing (and persistence on my side) found I had thyroid issues as well as polycystic ovary syndrome (PCOS) and insulin resistance. I started on some medications and my husband, Tyler, and I embarked on a major lifestyle change through the ketogenic diet. Many of my providers and supporters told me “lose weight and you’ll get pregnant.” I lost 100 lbs and call this *BS*; it’s a cop-out on your providers’ end by telling you that it’s your fault and they are unwilling to delve into the actual problem.
We gave our lifestyle changes 6 months before seeing a provider at an OB/GYN clinic. They talked about trying a few “Clomid cycles” but were still unable to give me much for answers to why this wasn’t working out for us or order any additional work-ups. That summer, we signed up to meet with a fertility clinic for a consultation (shout out to Dr. Conway and the treatment team at Idaho Fertility Center). Our reproductive endocrinologist was so lovely; she listened to our story and began ordering numerous tests to try to find out what was going on. My blood work confirmed the above issues with my thyroid and PCOS/IR, and also uncovered numerous irregularities in my hormones (namely estrogen, progesterone, testosterone, LH, and FSH). My weight was no longer a problem. We were young and our genetic testing showed no concerns. We did additional imaging that showed likely endometriosis and/or adenomyosis but no blockages. Tyler and I allowed ourselves an additional 6 months as we were still working on getting healthy and hoping that my hormones would level out.
We continued to be unsuccessful in getting pregnant so returned to the clinic and began the more grueling part of our journey. We started with a basic timed intercourse cycle; this entailed close imaging/monitoring and oral meds with a few belly shots to grow follicles, release an egg, then fertilize and implant based on a very specific timed schedule. Unfortunately, this ended in a chemical pregnancy. We did do additional imaging and found I had polyps and a fibroid that could possibly be impacting the ability for fertilized eggs to attach and implant in my uterus. After those findings, I went on to have a hysteroscopy and a polypectomy. The team decided my fibroid was likely not intruding enough into my endometrial lining to cause problems with implantation. Due to my poor results and minimal response to our medication protocol during the timed intercourse cycle, it was suggested we move on to intrauterine insemination (IUI) cycles. This process was quite similar in terms of oral medications, injections, and close monitoring, followed by a noninvasive procedure of inserting a catheter with the sperm through the cervix and hoping timing would be on our side. Unfortunately, all 3 IUIs failed.
At this point, we reconvened with the reproductive endocrinologist to discuss our next steps. She highly recommended moving towards in vitro fertilization, or IVF, with the suggestion that we do frozen embryo transfers rather than fresh due to my body’s struggle with managing both ovaries and uterus at the same time as well as their slightly higher rate of success. I was asked to stop losing weight and actually GAIN some (after all that work, that was incredibly hard to hear!) After discussion and lots of prayer, we decided to do back-to-back egg retrievals with ICSI (sperm is directly inserted into the egg) and a “freeze all.” Each egg retrieval consisted of 3-6 injections per day, topical and oral meds, and very close imaging and blood work monitoring.
 Typically you are “stimming” (hyper-stimulating your ovaries to make and mature as many follicles as possible) for about 10 days: round one required me to stim for 14 days, our second round only 11 days. In those last few days of each cycle, I went into the clinic every day to measure follicle size and complete blood work to find out if we would “trigger” (an injection that initiates the final maturation and release of the follicles/eggs). Once triggered, a retrieval would happen 36 hours afterward.
Typically you are “stimming” (hyper-stimulating your ovaries to make and mature as many follicles as possible) for about 10 days: round one required me to stim for 14 days, our second round only 11 days. In those last few days of each cycle, I went into the clinic every day to measure follicle size and complete blood work to find out if we would “trigger” (an injection that initiates the final maturation and release of the follicles/eggs). Once triggered, a retrieval would happen 36 hours afterward.
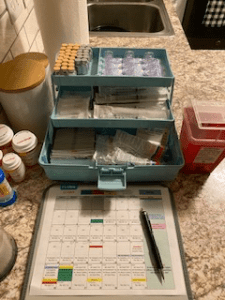 For the retrieval procedure, I was put under general anesthesia while the doctor inserted a long needle through the cervix and into each ovary to carefully extract the mature follicles/eggs. After the eggs were extracted, they were injected with the best sperm and allowed 3-6 days to fertilize, turn to blastocysts, and then frozen. During both retrievals, my medication protocol was adjusted multiple times to achieve better results.
For the retrieval procedure, I was put under general anesthesia while the doctor inserted a long needle through the cervix and into each ovary to carefully extract the mature follicles/eggs. After the eggs were extracted, they were injected with the best sperm and allowed 3-6 days to fertilize, turn to blastocysts, and then frozen. During both retrievals, my medication protocol was adjusted multiple times to achieve better results.
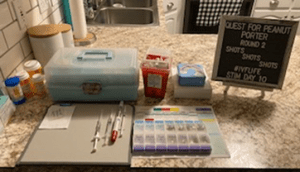 On our first retrieval, 13 eggs were retrieved, 9 fertilized, and 2 made it to 5-day blastocyst stage (graded at a BB and BC). For round 2, 16 were retrieved, 13 fertilized, and 1 made it on day 5 and 2 additional made it to blastocysts stage by day 6 (BA, BB, BC). This was Arlo’s batch, she’s our sweet little 5-day BA embryo. We chose not to do any genetic testing on our embryos.
On our first retrieval, 13 eggs were retrieved, 9 fertilized, and 2 made it to 5-day blastocyst stage (graded at a BB and BC). For round 2, 16 were retrieved, 13 fertilized, and 1 made it on day 5 and 2 additional made it to blastocysts stage by day 6 (BA, BB, BC). This was Arlo’s batch, she’s our sweet little 5-day BA embryo. We chose not to do any genetic testing on our embryos.
[easy-image-collage id=16662]
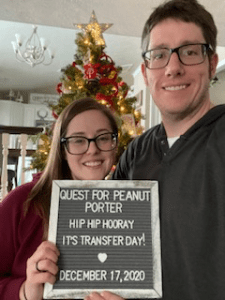 I was able to take a brief, 1-month long reprieve before jumping into our first frozen embryo transfer. This consisted of oral meds and a daily injection of PIO (progesterone in oil…a 22 gauge 1½” needle…in the butt…) We had daily to every other day monitoring to assess the thickness of my endometrial lining and hormone levels to be sure we were giving the embryo the best chance at sticking. The procedure for this was much less invasive. An embryo was removed from the cryo vault, thawed (with fingers crossed that the embryo would survive the thawing process), then inserted through the cervix into my uterus using a catheter. I did acupuncture both right before and right after the procedure, partook in the traditional/superstitious McDonald’s French fries, then spent the next 3 days taking full advantage of my “princess days.”
I was able to take a brief, 1-month long reprieve before jumping into our first frozen embryo transfer. This consisted of oral meds and a daily injection of PIO (progesterone in oil…a 22 gauge 1½” needle…in the butt…) We had daily to every other day monitoring to assess the thickness of my endometrial lining and hormone levels to be sure we were giving the embryo the best chance at sticking. The procedure for this was much less invasive. An embryo was removed from the cryo vault, thawed (with fingers crossed that the embryo would survive the thawing process), then inserted through the cervix into my uterus using a catheter. I did acupuncture both right before and right after the procedure, partook in the traditional/superstitious McDonald’s French fries, then spent the next 3 days taking full advantage of my “princess days.”
 After the procedure, you have the dreaded “2-week wait (TWW)” before you get your “Beta HCG” (pregnancy blood test) to confirm success. For this test, they look for anything over 100; my levels were at 332! We were officially pregnant!! Over the course of the next few weeks, we continued to get blood work and early imaging to assess viability; each appointment was met with anxiety but then increased hope. At 9 weeks, we were officially graduated from the fertility clinic (for this round) and moved on to regular OBGYN care.
After the procedure, you have the dreaded “2-week wait (TWW)” before you get your “Beta HCG” (pregnancy blood test) to confirm success. For this test, they look for anything over 100; my levels were at 332! We were officially pregnant!! Over the course of the next few weeks, we continued to get blood work and early imaging to assess viability; each appointment was met with anxiety but then increased hope. At 9 weeks, we were officially graduated from the fertility clinic (for this round) and moved on to regular OBGYN care.
An IVF pregnancy is not automatically a high-risk pregnancy and should be treated as any other pregnancy unless you have other underlying issues. You are at higher risk of pre-eclampsia, but I never had issues with this. Overall, my pregnancy, labor, and delivery were lovely and relatively uncomplicated.
[easy-image-collage id=16663]
Infertility and IVF is a hard, lonely journey, and I wouldn’t wish it on anyone. But we are so incredibly grateful for the opportunity to expand our family and for the amazing resources available in this day and age (and LOCAL!)
For those of you that stuck through to the very end of this long story, thank you!













